For healthcare organizations and insurance companies alike, implementing robust medical insurance claims processing has become not just beneficial but essential for survival. This is because claim denials and rejections remain a persistent challenge in revenue cycle management, cited in fact, as the biggest challenge in 2024 [Plutus Health RCM Challenges Index].
Mastering the strategies for effective claim denial management can mean the difference between a thriving practice and one struggling to maintain financial stability. This article attempts to help you establish such a mechanism and reduce claim denial rates.
Page Contents
The Difference between Claim Denials and Claim Rejections
Claim denial happens at the payer’s end (the insurance company). After the insurance company reviews the claim and processes it, they deny payment based on issues related to policy coverage, lack of medical necessity, or other policy-related reasons.
Claim rejection happens before the claim is fully processed. It happens at the healthcare provider’s end, before the claim reaches the payer for review. It is typically due to errors in claim submission, such as incorrect patient information, coding errors, or missing documentation. Once corrected, the claim is submitted to the insurance company for processing.
How Does Medical Claims Denial Management Work?
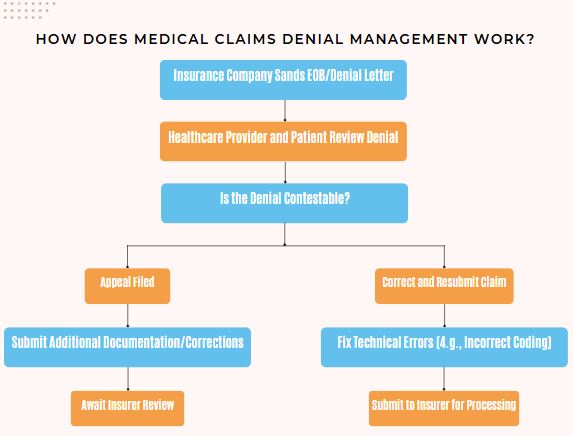
The insurance company sends an Explanation of Benefits (EOB) or denial letter to both the healthcare provider and the patient, outlining the reason(s) for the denial. This document is used to understand the reason for denial.
If the denial is contestable (e.g., medical necessity or incorrect decision), an appeal is filed with the insurance company, providing additional documentation, medical records, or corrections to support the case. If the denial is due to a technical error (e.g., incorrect coding), the claim can be corrected and resubmitted without a formal appeal.
Why is Denial Management Equally Crucial for Healthcare Providers and Insurance Firms?

Source: Experian
At the end of the day, both healthcare and insurance companies have to ensure optimized revenue cycle management.
- Healthcare firms must ensure accurate claim submissions and appeal all denied claims in time to recover revenue that will otherwise be lost.
- Insurance firms must ensure that all the claims comply with their policy guidelines, that only valid claims are paid out, and that all incoming appeals are managed judiciously.
Effective medical claims denial management helps reduce revenue loss, and therefore, it is equally critical for a healthcare firm and an insurance company.
Furthermore, proactive denial management (i.e., identifying patterns in claim denials to correct issues and prevent future denials) ensures cash flow stability, reduces the risk of legal complications or penalties, and minimizes administrative burdens.
The Fundamentals of Effective Claim Denial Management
Let’s examine the fundamental components of denial management in healthcare and insurance domains that can help optimize your revenue cycle.
- Identify and Understand Reasons for Claim Denials
Claim denials are revenue cycle management’s greatest challenge, with more than 1 in 5 providers saying they lose $500K in annual revenue because of denials. Borrowed from the latest Plutus Health Revenue Cycle Management Challenges Index, this data indicates a pressing need for understanding why the claims are denied and proactively acting on them.
There are various reasons why claims might be denied, but some of the most common ones include:
- Incomplete or Incorrect Information: Claims are missing essential details like patient name, ID number, or service date.
- Medical Billing or Coding Errors: Incorrect use of CPT or ICD-10 codes can lead to claim rejections.
- Lack of Coverage: The service, treatment, or procedure isn’t covered under the patient’s insurance policy.
- Doubt over Medical Necessity: The insurer declares the treatment or procedure not medically necessary based on their policies/guidelines.
- Preauthorization Required: The treatment required prior authorization, but it wasn’t obtained before the service was provided.
- Out-of-Network Provider: The provider who rendered the service is out of the patient’s insurance network.
- Duplicate Claim: A similar claim has already been submitted and processed.
- Expired Filing Time: The claim was submitted past the allowable period for claim submission
- Coordination of Benefits: The insurance company needs more information regarding other insurance coverage (e.g. when the patient has multiple insurance plans).
- Analyze and Categorize Denials
Once the denials are identified, it’s essential to categorize them by type—technical errors versus policy-related issues, for example. By analyzing denials, healthcare providers can pinpoint where the problem lies. A key aspect of denial management in healthcare is understanding which denials can be corrected and resubmitted and which require an appeal.
Consider categorizing denials by:
- Type (technical, clinical, administrative)
- Department
- Payer
- Dollar amount
- Frequency
For example, if your analysis reveals that 40% of denials stem from registration errors, you can focus resources on improving front-end processes and staff training in those specific areas. Or, if medical coding errors are a frequent issue, it might indicate the need for additional staff training or a review of the coding guidelines.
- Correct and Resubmit Claims
For claims that are rejected due to technical issues, such as coding or documentation errors, the next step is correcting and resubmitting them. The quicker a provider can identify and correct these errors, the faster they can receive payment. Promptly resubmitting corrected claims can help reduce the financial impact of denials.
For instance, this could involve-
- Ensuring that documentation accurately reflects the services provided
- Rechecking and using the appropriate ICD-10 codes for the diagnoses and procedures
- Confirming that the patient’s insurance coverage is active and valid
- Appeal Where Necessary
In cases where claims are hard denied and cannot be corrected through resubmission, an appeal is the next critical step. Unlike simple technical errors that can be quickly corrected and resubmitted, appealing a denied claim involves a more detailed and formal process. The appeal process involves submitting additional documentation, compelling evidence, and justification to support the claim’s validity.
For instance, if a claim for a specific surgical procedure is denied on the grounds that the insurance company considers it elective, the appeal would need to include medical records proving the urgency or necessity of the surgery.
A strong, well-supported appeal increases the chances of reversing the denial. At the same time, understanding payer-specific requirements is also vital here; some payers may allow up to a year for appeals, while others may have shorter timeframes. Missing this deadline often results in a lost opportunity for reimbursement, even if the appeal would have been successful.
Outsourcing Denial Management: Does It Help?
For Healthcare Firms
Outsourcing denial management in healthcare offers providers a strategic advantage in revenue cycle optimization. Specialized vendors offer dedicated teams with experienced personnel having deep expertise in payer policies, coding requirements, and regulatory compliance.
Key benefits include:
- Access to experienced denial tracking professionals
- Reduced operational costs compared to maintaining in-house teams
- Faster denial resolution due to focused resources
- Improved cash flow through faster reimbursements
- Regular analytics and reporting for process improvement
Moreover, outsourcing allows healthcare providers to focus on core clinical operations while experts handle the complex landscape of claims management and appeals.
For Insurance Firms
By partnering with specialized service providers, insurers can achieve more accurate claims processing. It also leads to better relationships with healthcare providers and improved member retention rates, while maintaining cost-effective operations.
Key benefits include:
- Reduced administrative burden on internal teams
- Enhanced compliance with regulatory requirements
- Faster claims turnaround times
- Better resource allocation during high-volume periods
- More consistent decision-making processes
While Claim Denials are Inevitable, their Impact isn’t
Whether you choose to build an in-house denial management team or partner with specialized medical claims processing service providers, the key is to act now. In an industry where every denied claim represents not just lost revenue but also delayed patient care and stagnant cash flow, effective claim denial management has become the cornerstone of successful operations.
Remember: The most successful healthcare organizations and insurance companies aren’t those that never face denials—they’re the ones that manage them most effectively.